Weight Loss Medications
30 December 2025 –
![]() Ernesto Escobar, MD
Ernesto Escobar, MD
The treatment of obesity has been categorically divided into two major groups:
Bariatric Surgery
Medications.
Within the bariatric surgery options, as previously discussed in the Blog, treatment requires intervention or modification of the digestive tract, either through laparoscopic surgery (minimally invasive) or endoscopic approaches (gastric balloon, gastric plication, etc.).
On this occasion, we will focus on the use of weight loss medications, which constitute a very diverse group.
Before going into detail, it is important to understand when the decision is made to opt for medications versus surgery. The most commonly used indications are as follows:
| Indication | Medications | Surgery |
|---|---|---|
| Body Mass Index (Without Diabetes) | 25–34.9 | a) 30–34.9 (selected cases) b) 35 or higher |
| Body Mass Index (With Type 2 Diabetes) | 25–29.9 | 30 or higher |
| Contraindications to Surgery | Yes | No |
The most commonly used medications for weight loss can be classified based on their route of administration and mechanism of action:
Oral (tablets, capsules)
-
Phentermine (Terfamex, Istaril): decreases appetite by acting on the central nervous system and increases metabolism.
-
Amfepramone (Neobes, Norex): decreases appetite by acting on the central nervous system and increases metabolism.
-
Orlistat (Andanza): acts at the gastrointestinal level by inhibiting fat digestion; it may cause diarrhea and fecal incontinence.
-
Natural extracts.
Injectable
-
Semaglutide (Ozempic)
-
Liraglutide (Saxenda, Victoza)
-
Tirzepatide (Mounjaro)
-
Dulaglutide (Trulicity)
-
Exenatide (Byetta)
-
Extended-release Exenatide (Bydureon BCise)
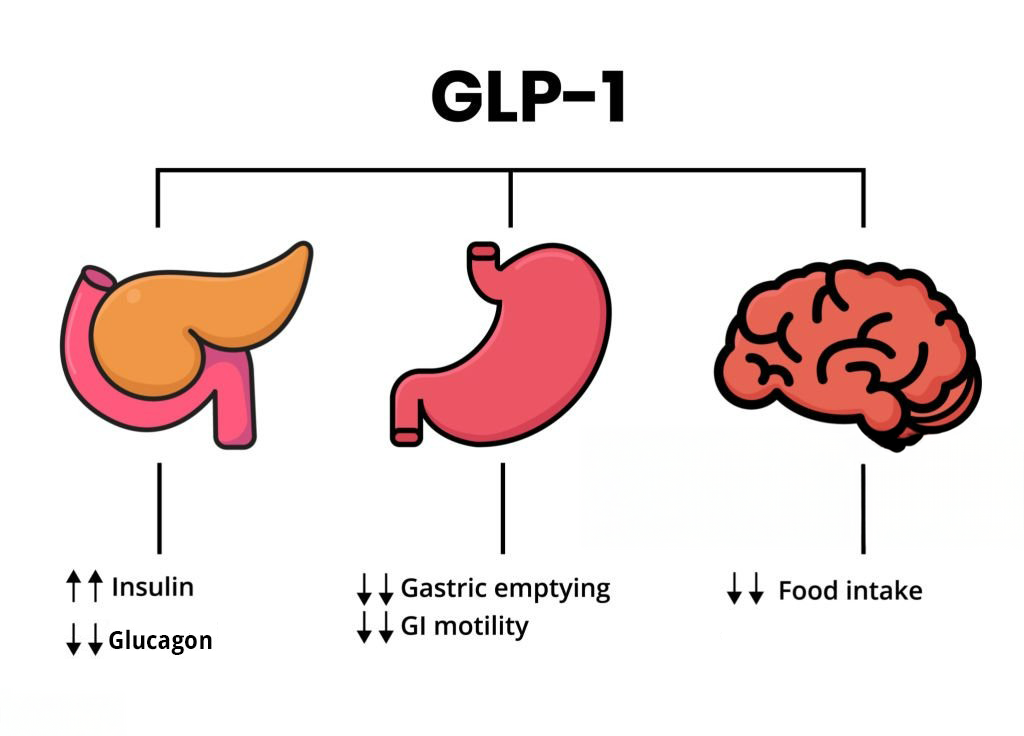
These medications act on receptors of a hormone known as GLP-1, which enhances insulin sensitivity.
Oral medications are significantly less expensive than other treatment options; however, they are most effective in cases of overweight (BMI 25–29.9) and Class I obesity (BMI 30–34.9).
Several factors must be considered before prescribing them, including the patient’s overall health status, cardiovascular disease, type 2 diabetes, or other conditions that may contraindicate their use or instead favor surgical treatment.
Injectable medications act by mimicking the effect of a natural hormone produced in the small intestine in response to food intake, called GLP-1 (Glucagon-Like Peptide-1). This hormone enhances insulin response by increasing cellular sensitivity, resulting in improved blood glucose control.
This mechanism explains why hospitalized patients with type 2 diabetes who are eating during hospitalization maintain better glycemic control compared to those who are fasting and receiving only intravenous fluids.
Once GLP-1 was identified as beneficial for diabetes control, synthetic analogs were developed to replicate its effects. These medications are marketed as GLP-1 receptor agonists, with the most well-known brands being Ozempic, Victoza, Saxenda, and Mounjaro.
Over time, it was observed that these medications also produce weight loss comparable to that achieved with Bariatric Surgery. This is explained by the fact that patients who undergo Gastric Bypass surgery experience increased natural production of GLP-1, representing an endogenous increase of this hormone.

Although injectable medications may result in significant weight loss, it is important to recognize that they are not harmless and may cause various adverse effects, including:
-
Nausea and vomiting
-
Diarrhea
-
Constipation
-
Abdominal pain and indigestion
-
Headache and dizziness
-
Allergic reactions or rash at the injection site
Other complications that have been documented in some cases include:
-
Pancreatitis
-
Loss of muscle mass (sarcopenia, “Ozempic face”)
-
Nutritional deficiencies
-
Taste disturbances
-
Renal injury/damage
Most Undesirable Effects
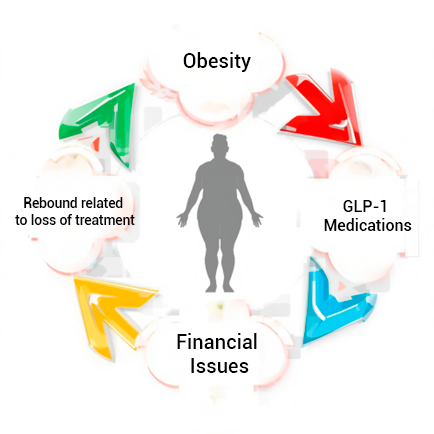
Financial burden: full-dose treatment represents a monthly cost of approximately USD $1,200 to $1,400.
Weight regain: although weight loss may be similar to that achieved with bariatric surgery, discontinuation of these medications leads to a rebound phenomenon (weight regain). In fact, the cost of 7 to 10 months of treatment often exceeds the cost of undergoing Bariatric/Metabolic Surgery at our Center.
Regarding weight regain or “rebound,” it is important to note that Bariatric/Metabolic Surgery may also present this phenomenon. However, it remains the option that offers the best long-term results, as not all patients can afford injectable medications on a long-term basis. Furthermore, the highest success rates of bariatric surgery are observed in patients who achieve appropriate lifestyle and dietary changes.
This does not mean that injectable medications do not have a defined role in obesity treatment. On the contrary, they are useful in combined therapies, such as adjuncts to endoscopic treatments in selected patient groups, or as adjuvant therapy for “bariatric plateau” or “bariatric rebound.”
At present, ongoing research is still determining which metabolic patient subgroup may benefit the most from this treatment modality, as this is an area being aggressively exploited by the pharmaceutical industry.
Finally, it must be noted that due to the ease of prescribing these medications, many non-surgical specialists are prescribing them indiscriminately. This has a significant economic impact and ultimately affects patient health, as it does not resolve obesity permanently and represents only a temporary solution.
